Do Face Masks Work? Peer-Reviewed Studies Show No Benefits Or Prevention Against Respiratory Illnesses
Denis G. Rancourt is a researcher at the Ontario Civil Liberties Association (OCLA.ca) and is formerly a tenured professor at the University of Ottawa, Canada. His paper titled “Masks Don’t Work A review of science relevant to COVID-19 social policy” includes scientific studies that shows ineffectiveness of facemasks in protecting of viral illnesses which was originally published at Rancourt's account on ResearchGate.net. As of June 5, 2020, this paper was removed from his profile by its admins at Researchgate.net/profile/D_Rancourt.
At Rancourt's blog ActivistTeacher.blogspot.com, he recounts the notification and responses he received from ResearchGate.net and states, “This is censorship of my scientific work like I have never experienced before.”
The original April 2020 white paper in .pdf format is available on this link : https://www.rcreader.com/sites/default/files/Denis%20G.%20Rancourt%20PhD%20April%202020%20%22Masks%20Don%27t%20Work%3A%20A%20review%20of%20science%20relevant%20to%20COVID-19%20social%20policy%22.pdf , complete with charts that have not been reprinted in the Reader print or web versions.
Research paper of Denis G,Rancourt starts with Summary :
“Masks and respirators do not work. There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles.
Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective-dose is smaller than one aerosol particle.
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.”
Below is a little summary of scientific studies (including ones from Denis G. Rancourt’s research paper) where study papers point to a lack of conclusive studies demonstrating the effectiveness of face masks in preventing viral infections. It’s also important to note that studies specifically examine all available peer reviewed papers on face masks efficacies; and they both unanimously state that no study established a conclusive relationship between mask/respirator use and protection against viral infections.
Moreover, as it can be seen from studies, negative and harmful side effects of mask usage remain undeniable. From headaches, skin reactions to hypoxemia, prolonged use of masks carries inescapable harmful consequences.
Furthermore, authorities around the world recommend we use cloth masks. On its face, considering the potential shortage of surgical and N95 masks, this recommendation seems reasonable. However, when we examine studies done specifically on cloth masks, we quickly realize not only do cloth masks offer almost no conclusive benefits against viral spreads (up to 97% particles penetration), usage of cloth masks may also introduce considerable risk of doing more harm than good. As demonstrated in studies, using cloth masks can actually make it more likely that someone would catch viral infections.
Besides, the entire premise of mask mandates rests upon the notion of ‘spread by asymptomatic SARS-CoV-2 carriers’; that asymptomatic SARS-CoV-2 carriers can and do spread the virus. Yet, we can see from study that infectivity of asymptomatic SARS-CoV-2 carriers appears anything but certain. In fact, the study could not find a single infection occurring among 455 contacts of asymptomatic COVID19 patients.
So, do masks really work? Should we all wear them? Judging from the peer-reviewed science documented above, no one in their right mind should make bold recommendations to use face masks; specially not cloth masks and definitely not for prolonged periods of time. And therefore, making them mandatory would simply seem insane to any sane person. Yet, governments mandate them. And due to surgical and N95 masks shortage, authorities, in essence, mandate cloth masks for millions around the world.
Even a large portion of the general public have been conditioned so effectively by the mainstream media and the medical authorities, that they often display a form of panic driven hysteria upon seeing someone not wearing a mask. Yet, anyone following legitimate published science can easily come to a very logical – and sensible – conclusion to not wear masks to prevent viral infections.
Therefore, instead of asking: do masks work? perhaps we should be asking: should masks be mandatory?
Review of the Medical Literature
Here are key anchor points to the extensive scientific literature that establishes that wearing surgical masks and respirators (e.g., “N95”) does not reduce the risk of contracting a verified illness:
Jacobs, J. L. et al. (2009) “Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial,” American Journal of Infection Control, Volume 37, Issue 5, 417 – 419. https://www.ncbi.nlm.nih.gov/pubmed/19216002
Conclusion: Face mask use in health care workers has not been demonstrated to provide benefit in terms of cold symptoms or getting colds. A larger study is needed to definitively establish noninferiority of no mask use. Face mask use in HCW was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
Acta Neurol Scand. 2006 Mar; 113(3): 199–202. Published online 2006 Jan 25. doi: 10.1111/j.1600-0404.2005.00560.x Headaches and the N95 face‐mask amongst healthcare providers https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7159726/
Conclusions: Healthcare providers may develop headaches following the use of the N95 face‐mask. Shorter duration of face‐mask wear may reduce the frequency and severity of these headaches. N95-masked health-care workers (HCW) were significantly more likely to experience headaches.
Cowling, B. et al. (2010) “Face masks to prevent transmission of influenza virus: A systematic review,” Epidemiology and Infection, 138(4), 449-456. https://www.cambridge.org/core/journals/epidemiology-and-infection/article/face-masks-to-prevent-transmission-of-influenza-virus-a-systematic- review/64D368496EBDE0AFCC6639CCC9D8BC05
In conclusion there remains a substantial gap in the scientific literature on the effectiveness of face masks to reduce transmission of influenza virus infection. While there is some experimental evidence that masks should be able to reduce infectiousness under controlled conditions [7], there is less evidence on whether this translates to effectiveness in natural settings. There is little evidence to support the effectiveness of face masks to reduce the risk of infection. Current research has several limitations including under powered samples, limited generalizability, narrow intervention targeting and inconsistent testing protocols, different laboratory methods, and case definitions. Further in-vivo studies of face masks in infectious individuals are warranted to determine the proportion of exhaled virus that is trapped by the mask.
None of the studies reviewed showed a benefit from wearing a mask, in either HCW or community members in households (H). See summary Tables 1 and 2 therein.
bin-Reza et al. (2012) “The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence,” Influenza and Other Respiratory Viruses 6(4), 257–267. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1750-2659.2011.00307.x
In conclusion, there is a limited evidence base to support the use of masks and ⁄ or respirators in healthcare or community settings. Mask use is best undertaken as part of a package of personal protection, especially including hand hygiene in both home and healthcare settings. Early initiation and correct and consistent wearing of masks ⁄ respirators may improve their effectiveness. However, this remains a major challenge – both in the context of a formal study and in everyday practice. Continued research on the effectiveness masks ⁄ respirators use and other closely associated considerations remains an urgent priority with emphasis being on carefully designed observational studies and trials best conducted.
“There were 17 eligible studies. … None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”
· Smith, J.D. et al. (2016) “Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis,” CMAJ Mar 2016 https://www.cmaj.ca/content/188/8/567
Conclusion : Although N95 respirators appeared to have a protective advantage over surgical masks in laboratory settings, our meta-analysis showed that there were insufficient data to determine definitively whether N95 respirators are superior to surgical masks in protecting health care workers against transmissible acute respiratory infections in clinical settings.
“We identified six clinical studies … . In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
· Offeddu, V. et al. (2017) “Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis,” Clinical Infectious Diseases, Volume 65, Issue 11, 1 December 2017, Pages 1934–1942, https://academic.oup.com/cid/article/65/11/1934/4068747
Conclusion: We found no clear benefit of either medical masks or N95 respirators against pH1N1… Overall, the evidence to inform policies on mask use in HCWs is poor, with a small number of studies that is prone to reporting biases and lack of statistical power
“Self-reported assessment of clinical outcomes was prone to bias. Evidence of a protective effect of masks or respirators against verified respiratory infection (VRI) was not statistically significant”; as per Fig. 2c therein:
Radonovich, L.J. et al. (2019) “N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial,” JAMA. 2019; 322(9): 824–833. https://jamanetwork.com/journals/jama/fullarticle/2749214
Conclusion: Among outpatient HCP, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza
“Among 2862 randomized participants, 2371 completed the study and accounted for 5180 HCW-seasons. ... Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.”
Long, Y. et al. (2020) “Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis,” J Evid Based Med. 2020; 1- 9. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381
“A total of six RCTs involving 9,171 participants were included. There were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection, and influenza-like illness using N95 respirators and surgical masks. Meta-analysis indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78). The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza.”
Objective: Previous meta-analyses concluded that there was insufficient evidence to determine the effect of N95 respirators
Conclusion: The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza. It suggests that N95 respirators should not be recommended for general public and nonhigh-risk medical staff those are not in close contact with influenza patients or suspected patients.
The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease - https://www.researchgate.net/publication/8371248_The_physiological_impact_of_wearing_an_N95_mask_during_hemodialysis_as_a_precaution_against_SARS_in_patients_with_end-stage_renal_disease
Objective: This study investigated the physiological impact of wearing an N95 mask during hemodialysis (HD) on patients with ESRD.
Results: Thirty nine patients (23 men; mean age, 57.2 years) were recruited for participation in the study. Seventy percent of the patients showed a reduction in partial pressure of oxygen (PaO2), and 19% developed various degrees of hypoxemia.
Conclusion: Wearing an N95 mask for 4 hours during HD significantly reduced PaO2 and increased respiratory adverse effects in ESRD patients.
Short-term skin reactions following use of N95 respirators and medical masks - https://onlinelibrary.wiley.com/doi/epdf/10.1111/cod.13601
Objective: To analyze the short-term effects of N95 respirators and medical masks, respectively, on skin physiological properties and to report adverse skin reactions caused by the protective equipment.
Results: Skin hydration, TEWL, and pH increased significantly with wearing the protective equipment. Erythema values increased from baseline. Sebum secretion increased both on the covered and uncovered skin with equipment-wearing.
Conclusions: This study demonstrates that skin biophysical characters change as a result of wearing a mask or respirator. N95 respirators were associated with more skin reactions than medical masks.
Cloth masks versus medical masks for COVID-19 protection - https://www.researchgate.net/publication/340579116_Cloth_masks_versus_medical_masks_for_COVID-19_protection
Objective: Global shortage of medical masks is a real and expanding problem. In turn, there is growing availability on the market of cloth masks. This is a study on the comparison of the efficacy of cloth masks to medical masks in the context of viral infections.
Results: Laboratory tests showed the penetration of particles through the cloth masks to be very high (97%) compared with medical masks (44%). A consequence of the above penetration is also a higher risk of critical care illness, the influenza- -like illness is more significant in the cloth mask group than in the medical mask. Moreover, the rate of confirmation of laboratory-confirmed viruses was also much higher for cloth masks than for medical masks or groups that did not wear any mask.
Conclusion: Cloth masks don’t protect as well as medical masks. Moreover, the physical properties of a cloth mask, reuse, the frequency and effectiveness of cleaning, and increased moisture retention, may potentially increase the infection risk, since, as it indicated by Osterholm et al. [7] the virus may survive on the surface of the face- masks. In this context self-contamination through repeated use and improper doffing is possible. Observations during SARS suggested double-masking and other practices increased the risk of infection because of moisture, liquid diffusion and pathogen retention [8].
A cluster randomised trial of cloth masks compared with medical masks in healthcare workers - https://www.researchgate.net/publication/275360639_A_cluster_randomised_trial_of_cloth_masks_compared_with_medical_masks_in_healthcare_workers
Objective: The aim of this study was to compare the efficacy of cloth masks to medical masks in hospital healthcare workers (HCWs). The null hypothesis is that there is no difference between medical masks and cloth masks.
Results: The rates of all infection outcomes were highest in the cloth mask arm, with the rate of ILI statistically significantly higher in the cloth mask arm…. Penetration of cloth masks by particles was almost 97% and medical masks 44%.
Conclusions: This study is the first RCT of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection.
A study on infectivity of asymptomatic SARS-CoV-2 carriers - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219423/
Objective: It is debatable whether asymptomatic COVID-19 virus carriers are contagious. We report here a case of the asymptomatic patient and present clinical characteristics of 455 contacts, which aims to study the infectivity of asymptomatic carriers.
Results: The median contact time for patients was four days and that for family members was five days…. The blood counts in most contacts were within a normal range. All CT images showed no sign of COVID-19 infection. No severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections was detected in 455 contacts by nucleic acid test.
Conclusion: In summary, all the 455 contacts were excluded from SARS-CoV-2 infection and we conclude that the infectivity of some asymptomatic SARS-CoV-2 carriers might be weak.
· Preliminary report on surgical mask induced deoxygenation during major surgery* - http://scielo.isciii.es/pdf/neuro/v19n2/3.pdf
Objectives. This study was undertaken to evaluate whether the surgeons' oxygen saturation of hemoglobin was affected by the surgical mask or not during major operations.
Results. Our study revealed a decrease in the oxygen saturation of arterial pulsations (SpO2 ) and a slight increase in pulse rates compared to preoperative values in all surgeon groups. The decrease was more prominent in the surgeons aged over 35.
Conclusions. Considering our findings, pulse rates of the surgeon's increase and SpO2 decrease after the first hour. This early change in SpO2 may be either due to the facial mask or the operational stress. Since a very small decrease in saturation at this level, reflects a large decrease in PaO2 , our findings may have a clinical value for the health workers and the surgeons.
Considering our findings, this is the first clinical investigation reporting a decrease in blood O2 saturation and an increase in pulse rates of the surgeons after the operations due to surgical mask usage.
Research paper of Denis G,Rancourt ends with some very good points :
Why There Can Never Be an Empirical Test of a Nation-Wide Mask-Wearing Policy
As mentioned above, no study exists that shows a benefit from a broad policy to wear masks in public. There is good reason for this. It would be impossible to obtain unambiguous and bias-free results [because]:
1. Any benefit from mask-wearing would have to be a small effect, since undetected in controlled experiments, which would be swamped by the larger effects, notably the large effect from changing atmospheric humidity.
2. Mask compliance and mask adjustment habits would be unknown.
3. Mask-wearing is associated (correlated) with several other health behaviors; see Wada (2012).
4. The results would not be transferable, because of differing cultural habits.
5. Compliance is achieved by fear, and individuals can habituate to fear-based propaganda, and can have disparate basic responses.
6. Monitoring and compliance measurement are near-impossible, and subject to large errors.
7. Self-reporting (such as in surveys) is notoriously biased, because individuals have the self-interested belief that their efforts are useful.
8. Progression of the epidemic is not verified with reliable tests on large population samples, and generally relies on non-representative hospital visits or admissions.
9. Several different pathogens (viruses and strains of viruses) causing respiratory illness generally act together, in the same population and/or in individuals, and are not resolved, while having different epidemiological characteristics.
Unknown Aspects of Mask Wearing
Many potential harms may arise from broad public policies to wear masks, and the following unanswered questions arise:
1. Do used and loaded masks become sources of enhanced transmission, for the wearer and others?
2. Do masks become collectors and retainers of pathogens that the mask wearer would otherwise avoid when breathing without a mask?
3. Are large droplets captured by a mask atomized or aerolized into breathable components? Can virions escape an evaporating droplet stuck to a mask fiber?
4. What are the dangers of bacterial growth on a used and loaded mask?
5. How do pathogen-laden droplets interact with environmental dust and aerosols captured on the mask?
6. What are long-term health effects on HCW, such as headaches, arising from impeded breathing?
7. Are there negative social consequences to a masked society?
8. Are there negative psychological consequences to wearing a mask, as a fear-based behavioral modification?
9. What are the environmental consequences of mask manufacturing and disposal?
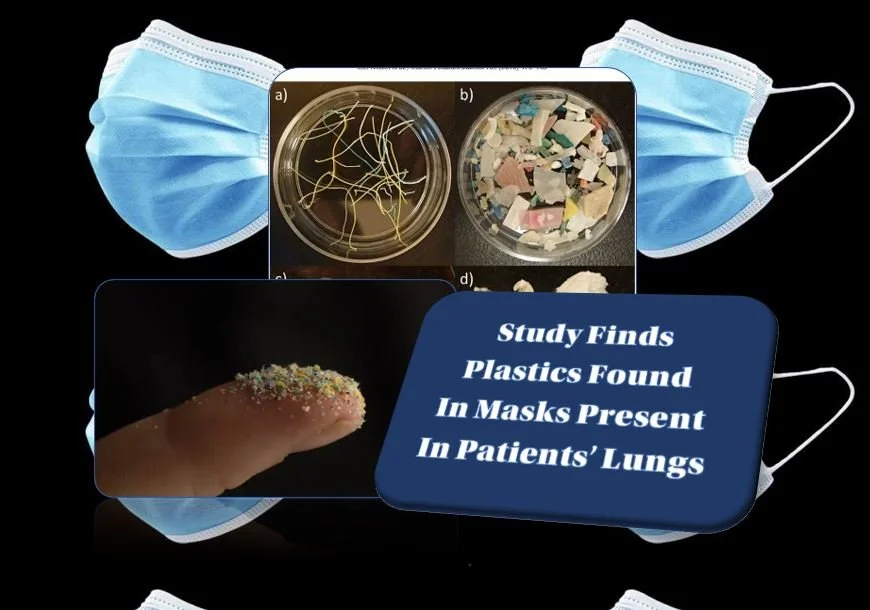
10.Do the masks shed fibers or substances that are harmful when inhaled?
Conclusion
By making mask-wearing recommendations and policies for the general public, or by expressly condoning the practice, governments have both ignored the scientific evidence and done the opposite of following the precautionary principle.
In an absence of knowledge, governments should not make policies that have a hypothetical potential to cause harm. The government has an onus barrier before it instigates a broad social-engineering intervention or allows corporations to exploit fear-based sentiments.
Furthermore, individuals should know that there is no known benefit arising from wearing a mask in a viral respiratory illness epidemic, and that scientific studies have shown that any benefit must be residually small, compared to other and determinative factors.
Otherwise, what is the point of publicly funded science?
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
Watch videos with Denis Rancourt:
COVID-19 And Face Masks- Interview with Ph.D Denis Rancourt (Dr Mercola)
Denis Rancourt - Argument Against Facemasks That Are Ineffective In Preventing Viral Transmission[Former Full Professor Of Physics At Ottawa University]
The CDC itself has said masks don’t work for similar sized viruses like influenza
Nonpharmaceutical Measures for Pandemic Influenza IN Nonhealthcare Settings— Personal Protective and Environmental Measures - https://wwwnc.cdc.gov/eid/article/26/5/19-0994_article
Facemasks:
· In pooled analysis, we found no significant reduction in influenza transmission with the use of face masks (RR 0.78, 95% CI 0.51–1.20; I2 = 30%, p = 0.25) (Figure 2). One study evaluated the use of masks among pilgrims from Australia during the Hajj pilgrimage and reported no major difference in the risk for laboratory-confirmed influenza virus infection in the control or mask group(33).
· The overall reduction in ILI or laboratory-confirmed influenza cases in the face mask group was not significant in either studies (9,10).
· … another study evaluated face mask use as a source control for infected persons only (35), and the remaining studies provided masks for the infected persons as well as their close contacts (11–13,15,17).
· Disposable medical masks (also known as surgical masks) are loose-fitting devices that were designed to be worn by medical personnel to protect accidental contamination of patient wounds, and to protect the wearer against splashes or sprays of bodily fluids (36). There is limited evidence for their effectiveness in preventing influenza virus transmission either when worn by the infected person for source control or when worn by uninfected persons to reduce exposure. Our systematic review found no significant effect of face masks on transmission of laboratory-confirmed influenza.
Watch the video When Dr. Fauci Said People Should Not Be Wearing Masks:
Denmark Study Finds Masks Are Ineffective
The first randomized controlled trial1,2 to assess the effectiveness of surgical face masks against SARS-CoV-2 infection specifically — which journals initially refused to publish — is finally seeing the light of day.
The so-called “Danmask-19 Trial,” published November 18, 2020, in the Annals of Internal Medicine,3 included 3,030 individuals assigned to wear a surgical face mask and 2,994 unmasked controls. Of them, 80.7% completed the study.
To qualify, participants had to spend at least three hours per day outside the home and not be required to wear a mask during their daily work. At the end of the study, participants reported having spent a median of 4.5 hours per day outside the home.
For one month, participants in the mask group were instructed to wear a mask whenever they were outside their home. Surgical face masks with a filtration rate of 98% were supplied. In accordance with recommendations from the World Health Organization, participants were instructed to change their mask after eight hours.
Antibody testing was performed before the outset and at the end of the study period. At the end of the month, they also submitted a nasal swab sample for PCR testing.
What the Danmask-19 Trial Found
The primary outcome was a positive PCR test, a positive antibody test result (IgM or IgG) during the study period, or a hospital-based diagnosis of COVID-19. Secondary end points included PCR evidence of infection with other respiratory viruses.
Based on the adherence scores reported, 46% of participants always wore the mask as recommended, 47% predominantly as recommended and 7% failed to follow recommendations. So, what did they find? As you might expect, there’s a reason why the researchers had such a hard time getting this study published:
Among mask wearers, 1.8% (42 participants) ended up testing positive for SARS-CoV-2, compared to 2.1% (53) among controls. When they removed the people who reported not adhering to the recommendations for use, the results remained the same — 1.8% (40 people), which suggests adherence makes no significant difference.
1.4% (33 participants) tested positive for antibodies compared to 1.8% (44) of controls.
Among those who reported wearing their face mask “exactly as instructed,” 2% (22 participants) tested positive for SARS-CoV-2 compared to 2.1% (53) of the controls.
52 participants in the mask group and 39 in the control group reported COVID-19 in their household. Of these, two participants in the mask group and one in the control group developed SARS-CoV-2 infection — a finding that suggests “the source of most observed infections was outside the home.”
0.5% (nine participants) in the mask group and 0.6% (11 individuals) tested positive for one or more respiratory viruses other than SARS-CoV-2 (secondary outcome).
All in all, this landmark COVID-19-specific study failed to deliver good news to those who insist face masks are a crucial component of the pandemic response. Masks may reduce your risk of SARS-CoV-2 infection by as much as 46%, or it may increase your risk by 23%. In other words, the preponderance of evidence still shows that masks have virtually no impact on viral transmission.
Some insist on following:
“even if masks are only one percent effective, that is still significant, when one is talking about a life and death situation for millions of people. At some point, we have to admit that we are at war, and anything that gives us any kind of an edge over the enemy is worth doing.”
This is faulty logic if masks are, in fact, spreading germs in the general public.
The whole premise is based on if healthcare workers do, so if it’s good for them it must be good for the general public.
The underlying facts are that healthcare workers dispose of their masks after EVERY use and they do NOT wear them to prevent “transmission”- they wear them to avoid sprays and droplets.
This action by professional healthcare workers does not translate to a germ ridden general public who touch their purses, touch the mask, touch their steering wheels, touch the mask, touch the shopping carts, touch the mask, touch public bathroom door handles and touch the mask and then… PUT THE MASK UP AGAINST THEIR MOUTH.
Even the package box for facemasks shows following:
Watch more videos on same topic:
WHAT W.H.O SUGGESTS ABOUT FACEMASK WEARING
WHO Told Us: “No Evidence To Suggest Wearing Masks Has Any Particular Benefits - Some Evidence Suggest Opposite"
WHO Told Us No Need To Wear A Facemask Unless Sick (March 2020) - Video That WHO Took Down Now From Their Website
FACEMASKS BEING MADE IN VERY UNHYGIENIC CONDITIONS
How Face Masks Are Being Made in India On A Dirty Floor
NEGATIVE IMPACT OF WEARING FACEMASKS ON PSYCHOLOGICAL, MENTAL AND SOCIAL LEVEL
Facemasks Will Cripple Society - The Face Mask Pandemic